MEIBOMIAN GLAND DYSFUNCTION (MGD)
Links to the pages
GLIMPSE on ... MGD
SUMMARY (Every sentence here is LINKED to a respective CHAPTER below)
Meibomian Gland Dysfunction (MGD), the most frequent alteration of the lipid producing Glands inside the eye lids, is the main causative factor for Dry Eye Disease. Members of the Ocular Surface Center Berlin (OSCB) have served as members and chair in the TFOS MGD Workshop Sub-Committee on Anatomy, Physiology and Pathophysiology of the Meibomian Gland. According to the present knowledge, MGD is a mainly obstructive gland alteration that leads to a deficiency in the amount and/ or the quality of the produced lipids and thus to a lipid deficiency of the Tear Film. This results in increased evaporation of water from the tear FILM and in an instability of the indispensable film of tears, that covers the ocular surface in the lid aperture. The subsequent increased friction and hyper-osmolarity of the remaining low tear volume induces damage of the ocular surface tissue ... altogether this represents Dry Eye Disease of its main evaporative type. Evaporative Dry Eye Disease is the main type of Dry Eye and MGD is, according to the presently available data, the main causative factor for Dry Eye Disease.
The two main factors in the pathophysiology of the disease process of obstructive MGD are Increased Viscosity of the Meibomian oily secretum and a Hyper-Keratinization of the Epithelium on the Lid Margin and inside the terminal duct and orifice of the Meibomian Glands. Typical clinical SIGNS for MGD are the Obstruction of the orifices by inspissated secretum that is still inside the glands or protrudes outside through the orifice as well as whitish to yellowish lipid material on the lid margin or whitish foam on the tear film and lid margin.
The typical pathologies of inspissated secretum and lipid debris on the lid margin are the RATIONALE for the application of PHYSICAL THERAPY APPROACHES such as Lid Warming, Gland Expression and Lid Margin Hygiene. Non-Obvious MGD (NOMGD) has no symptoms and the lid looks normal - but may still cause unnoticed gland destruction.
INTERNAL and EXTERNAL Negative INFLUENCE FACTORS (RISK FACTORS) such as e.g. endocrine imbalance, systemic skin disease, or contact lens wear and conjunctival inflammation play a ROLE in MGD. BACTERIAL COLONIZATION with mainly commensal species has an important role in MGD. Some THERAPY Options for Meibomian Gland Dysfunction MGD are indicated here at the end ... as an overview a few pages further down in this MGD Section ... and in the Chapter for Therapy of Dry Eye Disease in general.
Meibomian Gland Dysfunction (MGD) is the main causative factor for Dry Eye Disease
Meibomian Gland Dysfunction, mostly known by its abbreviation as MGD, is probably best known today because of its importance for Dry Eye Disease - where lipid deficiency due tot MGD is the main causative factor.
This observation seems to be in contrast to the seemingly ´telling´ name of´DRY´ Eye Disease ... that implies a simple lack of water for the very complex dysfunction of the ocular surface that constitutes the most frequent pathologic condition in ophthalmological practice.
In fact, the lipid deficiency due to obstructive MGD, appears to represent the main causative primary factor according to the results that we evaluated and presented in the TFOS MGD Workshop REPORT in 2011. Since then the field of MGD, in clinics and basic science, in diagnostics as well as in therapy has made amazing advancements ... that have improved the life of the patient as well as of the clinician.
Contribution of The Ocular Surface Center Berlin (OSCB) to Meibomian Glands Dysfunction (MGD)
The Summary Figure of the TFOS MGD Workshop Report summarizes the main factors in the Pathophysiology of MGD - and thus explains, which pathogenetic factors contribute to the onset and worsening of MGD and how they interact in this process.
Members of the Ocular Surface Center Berlin (OSCB) have served as members and chair in the TFOS MGD Sub-Committee on the "Anatomy, Physiology and Pathophysiology" of Meibomian Gland dysfunction.
Apart from an analysis of own and published results on the histology of the Meibomian Glands in normal condition and in MGD, together with a plethora of physiological data, we had also unearthed the evidence that points to the conclusion that a primary Lack of Lipids at the Ocular Surface and Tear Film is causing Dry Eye Disease in about four fifths of Dry Eye Patients due to several studies.
A result of this Subcommittee is also the Summary Diagram that summarizes all the available information on the pathophysiological interactions in MGD - complex but not complicated.
What is Meibomian Gland Dysfunction ?
A DYSFUNCTION of the Meibomian Glands (MGD) leads, due to the LIPI-DEFICIENCY of the Tear FIlm, to EVAPORATIVE DRY EYE DISEASE - which is the most frequent form that is the primary causative factor in about four fifth of Dry Eye Patients..
Meibomian Gland Dysfunction is
a mainly OBSTRUCTIVE alteration of the lipid producing Meibomian glands with a consequent
downstream quantitative or qualitative LIPID-DEFICIENCY
as the main type of Tear Film Deficiency due to:
i.e. a lack of normal suitable lipid species
that not longer suffice to form a stable tear film with the ability to retard aqueous tear evaporation
of the Tear Film in the TEAR FILM LIPID LAYER
that leads to the following ´Secondary Pathogenetic Factors´ of Tear Film Deficiency
reduced stability of the tear film
increased evaporation of the aqueous main phase of the tears
with downstream
increased osmolarity
wetting deficiency,
short tear film break-up time
increased lubrication with increased mechanical friction
EVAPORATIVE DRY EYE DISEASE
... as depicted for ´TEAR FILM DEFICIENCY´in the HOLISTIC DYNAMIC CONCEPT for Dry Eye Disease - for details please see there
MGD is the main reason for onset of Dry Eye Disease
The Secondary Pathogenetic Factors in Tear Film Deficiency interact as explained in the section for ´Dry Eye Disease - Hierarchy of Pathogenetic Factors´, and as depicted in the diagram to the right.
Therefore, MGD does not only lead via lipid deficiency to Hyper-Evaporation and Hyper-Osmolarity but can also translate into all other secondary pathogenetic factors and can thus also lead to unstable visual acuity, Wetting defects with Dry Spots, Increased Friction and Chronic Mechanical Irritation.
The more the destruction proceeds the more the full blown picture of Dry Eye Disease with all factors comes into existence.
HOW ... does Meibomian Gland Obstruction occur ?
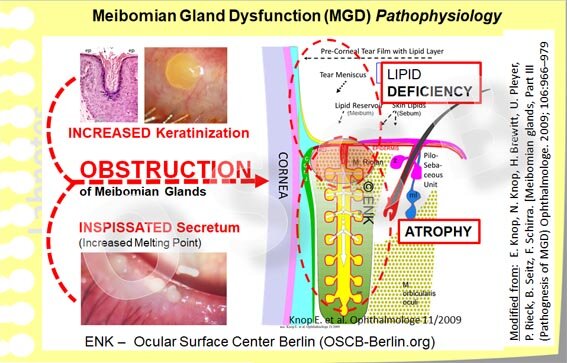
In a more focused an clinically oriented diagram, the two main PATHOGENETIC FACTORS that contribute to Meibomian Gland Dysfunction are shown together with the main CONSEQUENCES. Inspissated Meibomian Lipids, due to the occurrence of altered lipid species with increased melting point, and Hyperkeratinization of the Epithelium on the lid margin and inside the glands, can, together or alone, lead to obstruction of the Glands. The important downstream CONCEQUENCES are a (1) Lipid Deficiency on the lid margin and Tear Film with Tear Film Instability and Evaporative Dry Eye Disease. Also (2) an unnoticed pressure atrophy of the gland tissue inside the eye lids can occur due to the continuing production of oil. This leads to dilatation of the ducts and to atrophic destruction of the Secretory Meibocytes in the acini.
The two main factors in the pathophysiology of the disease process of obstructive MGD are
Increased Viscosity of the Meibomian oily secretum and a
Hyper-Keratini-zation of the Epithelium on the Lid Margin and inside the terminal duct and orifice of the Meibomian Glands that produces cornified squames that contribute to obstruct the lumen:
Underlying factors for the Pathophysiology in MGD
INCREASED VISCOSITY of the Meibomian lipid secretum
conceivably due to the influence of metabolic products such as lipolytic enzymes
produced by an increased colonization with the normal commensal bacterial species
together with
INCREASED EPITHELIAL KERATINIZATION (termed hyper-keratinization) due to
irritant lipid species or bacterial products or
soluble inflammatory mediators produce in the gland during sub-clinical inflammation
the influences of age
a lack of sufficient androgen sex hormone levels
or potential other factors
Typical SIGNS for MGD
Obstruction of the Meibomian Glands is typically easily detectable
In MGD the obstruction of the Meibomian Glands is typically detectable by inspissated secretum that is visible in one or the other way:
by a slight whitish protrusion of the orifice area
by inspissated secretum that is located still inside the gland but bulges the obstructed orifice outwards - this is termed pouting.
or by protrusions of inspissated secretum out of the orifice as a visible plug
similar to a cork that is half outside of the bottle - this is termed plugging.
In addition, there are other typical signs of MGD, such as
whitish foam on the tear film and lid margin from lipids altered by saponification
yellowish-brown lipid encrustations on the lid margin
similarly colored encrustations (collarettes) around the cilia of the anterior lid margin
redness of the lid margin, vascular protrusions as teleangiectasia, irregularity of the posterior lid border; in advanced cases displacement of orifices and lid margin rounding occur.
The typical pathologies of (1) inspissated obstructing secretum inside the gland and of (2) lipid debris on the lid margin are the RATIONALE for the application of PHYSICAL THERAPY APPROACHES:
WARMING of the Eye Lids is a general promising approach because of the inspissation of secretum due to lipids with increased melting point. Additional MOISTURE together with warming is another useful option, since hyper-keratinization is a co-factor for the obstructive process and also produces cornified squames and membrane-like structures on the lid margin that may be easier removed when they are moistened.
FORCEFUL ´THERAPEUTIC´ EXPRESSION of Meibomian Glands in order to remove the obstruction and to prevent further pressure atrophy of this gland with a certain chance, that this gland may re-normalize after one or repeated expressions during a longer follow up time. - The disadvantage is that forceful expression can be quite painful at times.
LID (Margin) HYGIENE is a procedure, where the lid margin is routinely cleaned with suitable, preferably lipid solutions or such that does not destroy lipids as this might negatively affect the tear film lipid layer. Lid Hygiene is applied twice daily, similar to tooth brushing, in order to remove accumulated lipid debris and bacterial contamination from the lid margin. This is best done after a gently massage of the eye lids in order to mobilize or express potential obstructions of Meibomian gland in order to also remove any material that was expressed from glands.
In NON-OBVIOUS Meibomian Gland Dysfunction (NOMGD) the lid margin appears typically quite normal (left) and this condition goes without symptoms because there is no effective deficiency of tear film lipids (yet). Only when mild pressure is applied to the lid margin in "Diagnostic Expression" it becomes obvious that no oil comes out of some Meibomian glands (middle). When strong pressure by a "Therapeutic" Expression is applied the inspissated secretum comes out of the orifices and it often has a toothpaste-like consistency (right - the redness here of the lid is due to the expression).
Non-Obvious MGD (NOMGD) has no symptoms and the lid looks normal - but may still cause unnoticed gland destruction
It becomes more tricky when obstructive MGD is not detectable - this is termed Non-Obvious MGD (NOMGD) - and the asymptomatic type may be more frequent than obvious MGD and is conceivably present in a majority of individuals - as explained in and article by Caroline BLACKIE and colleagues, where members of the Ocular Surface Center Berlin (OSCB) have also contributed.
In NOMGD there is an obstruction of Meibomian glands but typically the lid looks nornal and there are no symptoms because not all glands are affected so that there is still enough oil on the tear film. Still, according to the pathomechanism and the available histological studies on obstructed Meibomian glands it must be assumed that the gland tissue inside the eye lids is already undergoing a process or progressive pressure atrophy - as explained in more detail on the next page in the section for ´Overview on MGD´.
Non-Obvious MGD in normally appearing lids is a RATIONALE for "DIAGNOSTIC" Expression of the Meibomian Glands with minimal pressure roughly equivalent to the pressure that occurs during a blink. The aim is to check, whether a gland or a few of them along the lid margin, do indeed actively secrete oil ... which will then freely come out the orifice and cover it as a little lake of oil. This procedure was developed by Donald KORB and colleagues, is very easy and can simply be performed by mild digital pressure or by a specific instrument, the Meibomian Gland Evaluator (MGD) in order to always have a standardized pressure..
INTERNAL and EXTERNAL INFLUENCE FACTORS play a ROLE in MGD
INTERNAL Influence factors such as
age and sex, particularly the influence of sex hormones play an important role in the onset and progression of MGD.
Androgen deficiency that occurs generally more frequent in female sex and is more frequent with advancing age affects the Meibomian Glands similarly as the ocular surface in general .
in Androgen deficiency, the keratinization of the epithelium inside the glands and on the lid margin is up-regulated. Therefore hyper-keratinization, that decreases the width of the ducts and of the orifice, as one important pre-disposing factor in MGD, is typically worse in females and with advancing age.
Systemic disease, often skin disease such as seborrehic dermatitis and rosacea, as well of some therapy approaches, e.g. Isotretinoin (a Vitamin A derivate) that is used for acne therapy, has a negative effect on epithelial cells and promotes inflammatory pathways and MGD as observed by Juan DING and colleagues from David SULLIVANS group.
EXTERNAL INFLUENCE FACTORS
Contact Lens wear, independent of the type (rigid and soft), at least when the lenses are worn long term for many years apparently influences the Meibomian gland negatively. This causes MGD with destruction of gland tissue, detectable as drop-out in Meibography together with clinical deterioration of tear film parameters and symptoms of Dry Eye Disease as observed by Reiko ARITA and colleagues in Tokyo.
Inflammatory tarsal conjunctival disease in Ocular Allergy has the same effect as observed by the same group in another study.
Increased Bacterial Colonization of the lid margin and conceivably also ot the Meibomian Gland appears a an important pathogenetic factor in MGD. Bacterial colonization induces, via lipid degrading bacterial enzymes, the modification of the normal Meibomian lipids into irritant species that induce a chronic sub-clincal inflammatory process that is able to induce hyper-keratinization of the epithelium as an important risk factor for obstruction that leads to consequent stasis of secretum and thus re-inforces suitable conditions for a further increase of bacterial colonization. The described pathways constitute one important vicious circle for the chronicity of MGD.
Bacteria occur on the lid margin, similar to the skin, and also inside the Meibomian glands, as concluded from freshly expressed secretum by Joel DOUGHERTY from James McCULLEY´s group and they secrete lipid degrading enzymes that lead to irritant lipid species that reduce the tear film stability and induce a chronic inflammatory process in the Meibomian glands and the surrounding connective tissue.
Therefore it must be assumed that in MGD a chronic inflammatory process is ongoing, that is however sub-clinical and does typically in MGD not result in major clinical signs of inflammation.
THERAPY OPTIONS - for more detailed information => please see the section on ´Anti-Inflammatiory Therapy ´
Bacterial colonization with downstream inflammation as an important pathomechanism in MGD is a RATIONALE why systemic long-term therapy with tetracyclines (minocycline etc. ) is an established therapy approach in severe cases of MGD similar to blepharitis. The action is not so much an antibiotic one, as the typical dosage is too low, but ´side-effects´ are more important because tetracyclines also block the lipid degrading enzymes and have an anti-inflammatory component. Thereby a long-term normalization of the glands and the secretion is often achieved.
Another suitable pharmacon that combines an anti-bacterial effect together with a distinct anti-inflammatory action is azithromicin, a macrolide antibiotic. It has the advantages of short term efficacy and of storage within the tissue for long-term action. This allows effectiveness when applied only for a few days. Its primary indication at the ocular surface is infectious conjunctivitis but it has also proven great usefulness in the treatment of MGD - which is however outside the original indication.
Some THERAPY Options for Meibomian Gland Dysfunction MGD