OVERVIEW on ...
DRY EYE DISEASE
Dry Eye Disease is a complex, typically chronic, dysregulation of the functional anatomy of the ocular surface including the tear film that typically leads to symptoms of dryness, visual disturbance, ocular irritation and pain - it can be amplified by self-enforcing vicious circles that are prominently driven by inflammatory pathways and may eventually lead to a progressive destruction of the ocular surface.
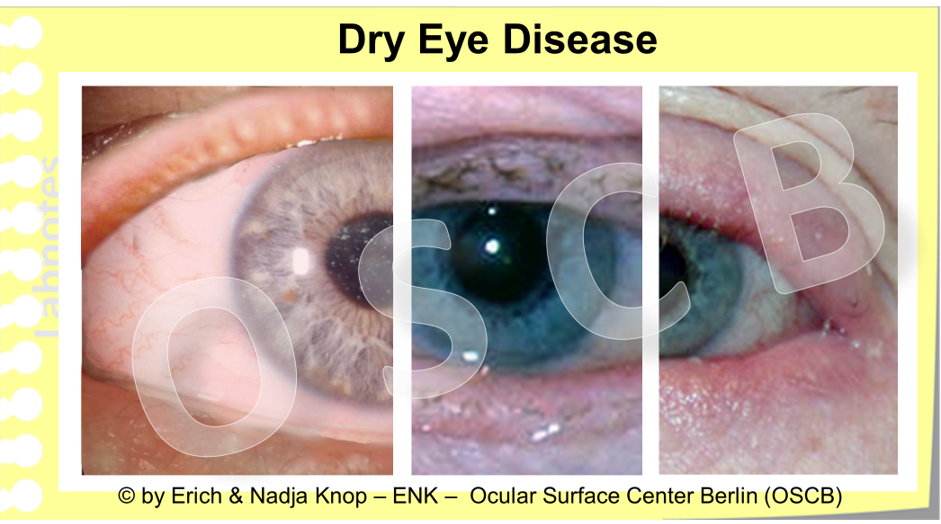
Some clinical images of patients with Dry Eye Disease - the disease severity increases from left to right including increasing alterations of the lid margin with pouting of Meibomian gland orifices, inflammation, lid margin rounding and irregularity, with loss of eye lashes
Dry Eye – a Syndrome or a Disease ?
The ´promiscuous´ nature of Dry Eye -its occurrence due to many different factors that impair wetting - may be the reason why it has long time been considered as a syndrome, i.e. a loosely related bunch of symptoms with unclear stringent etiology, rather than a disease with specific etiology.
This is similar to Sjögren´s Syndrome, the auto-immune inflammation of the lacrimal gland and other glands in the body, that is probably the best known, but still a practically rare, cause for aqueous-deficient Dry Eye. Sjögren´s Syndrome has meanwhile been ´officially promoted´ to a "Disease" ... for reasons that may be discussed, and Dry Eye ´Disease´ has also become an established term for valuable reasons.
In both of theses cases the scientific knowledge on the pathophysiology and therapy has greatly increased in recent years due to continuing and even increasing research efforts which may sufficiently justify the described development and which definitely supports many approaches for an evidence based therapy !
A valuable explanation for the ´promiscuous´ nature of Dry Eye, i.e. that it can occur due to many ´apparently´ underlying reasons - is probably the consideration that Dry Eye Disease in fact is ´a´ or ´the´ prototypic Disease of the Ocular Surface because:
Dry Eye occurs when various influence factors
eventually impair the most basic function of the Ocular Surface
ubiquitous/ complete and permanent MOISTURE
which is the basis for everything in terms of ´functions´ that comes later
It may be of interest to differentiate an occasional condition of ´ocular dryness´ or a "dry" eye that is easily overcome by removing or avioding desiccating conditions or by performing some forceful eye blinks from a chronic condition of where the ocular dryness is almost continuously present and is difficult to influence by the individual. Only the latter represents dry eye disease.
Dry Eye Disease is a Prototypic Ocular Surface Disease
Dry Eye Disease typically occurs ... after the MOIST has gone
Dry Eye Disease is a prototypic Ocular Surface Disease because it is based on a deficiency of Moisture - which is the most basic function of the Ocular Surface. Moisture is the pre-requisite for Ocular Surface Health and thus for the establishment and maintenance of vision ... as explained in the Ocular Surface Section.
Dry Eye Disease is a prototypic ocular surface disease because:
it is based on an impairment of the most basic function of the Ocular Surface - which is the maintenance of moisture
it can therefore be induced by a variety of factors and
it can affect all parts of the ocular surface unit
independent of the starting point …
and eventually,
the lack of moisture leads to onset of the signs and symptoms of Dry Eye Disease
Moisture is the pre-requisite for Ocular Surface Health and thus for the establishment and maintenance of vision
as long as the basic anatomical integrity of the tissues and organs is provided and
as long as the functional interaction of the organs is achieved ... as explained in the ´Ocular Surface´ Section (for details please see there).
Dry Eye Disease is non-specific in the sense that it is not specifically due to any particular infection or allergic or other specific affection of the ocular surface.
Some general systemic risk factors such as age, sex hormone levels or skin diseases increase the risk of Dry Eye Disease. Environmental factors can also play a significant role.
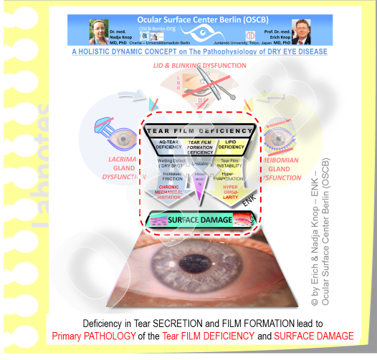
Dysfunctions in Tear SECRETION and in Tear FILM FORMATION are the Basic Causative Factors for the Onset of Dry Eye Disease
Dysfunctions in Tear SECRETION and in Tear FILM FORMATION are the Basic Causative Factors for the onset of Dry Eye Disease because they impair the ability of the Ocular Surface to provide a permanent moist coating in all zones, including the Cornea and Conjunctiva in the opened palpebral fissure ... which typically leads to Surface Tissue Damage.
Impairment of the Basic Functional Complexes of Ocular Gland SECRETION and Tear FILM FORMATIONmeans ...
... that the Ocular Surface can no longer provide the permanent moisture in the pre-ocular zone of the bulbar surface ...
... that lies in the lid aperture (palpebral fissure) where the Ocular Surface is exposed to the ambient dry environment.
When this situation becomes chronic, it necessarily leads to the development of Dry Eye Disease.
Various alterations of the Ocular GLANDS and of the Eye LIDS can be involved as CAUSATIVE FACTORS.
A deficiency in tear secretion of the ocular glands appears as the most frequent reason for Dry Eye Disease
The most frequent types of Dry Eye Disease are due to a deficiency of the lipid phase and of the aqueous phase. Even though the term Dry Eye Disease seems to imply that a loss of water must be more important, the main reason, according to the present data, is a primary deficiency of tear film lipids.
´Deficiency´ is a relatively general term because it describes quantitative and also qualitative deficiency of the secretion by the ocular glands.
A deficiency in tear secretion, of any kind, is the most frequent causative factor for Dry Eye Disease.
This explains the two main types of Dry Eye Disease due to tear film deficiency
the AQUEOUS deficient type and
the LIPID deficient/ evaporative type.
A primary deficiency of Tear Film lipids is the most frequent cause for Dry Eye Disease
Meibomian Gland Dsfunction (MGD) is the main reason for a deficiency of tear film lipids. In MGD there is a quantitative deficiency of lipids on the lid margin and tear film due to the gland obstruction. At the same time there is also a qualitative deficiency of lipids because hardened, opaque lipid species of increased melting point occur, as well as irritant free fatty acids with negative influence on the lid margin tissue and on the stability of the tear film.
In recent years it was found that the most frequent cause of Dry Eye is a lipid deficiency of the tear film. This occurs due to the mainly obstructive dysfunction of the Lipid-Producing Meibomian Glands in Meibomian Gland Dysfunction MGD (for details please see there).
Due to the obstructive process the amount of delivered lipids on the ocular surface and on the tear film is typically decreased which causes increased evaporation of the aqueous phase.
On the other hand, also the qualitative composition of the lipids is altered in disease, because
lipids with increased melting point are formed that contribute to the obstruction process of the gland duct and orifice
also irritant lipid species, such as free fatty acids, occur that may cause irritation of the lid margin tissue and decrease of the stability of the remaining tear film.
Desiccating Environmental Risk Factors can negatively influence the secreted tear fluid on the ocular surface
External Factors with negative influence on the tear fluid that is already secreted onto the Ocular Surface pose an increased risk for the onset and worsening of Dry Eye Disease. There are plenty of such risk factors in our daily private life and work environments.
This concerns every e.g. desiccating environments with high ambient temperature and a low humidity which both increase the rate of water evaporation from the Ocular Surface. Similarly higher wind speed as is intended by using fans in the summer have the same effect. Contact lenses have higher requirements for tear volume and may also increase the evaporation of tears.
Visual tasks such as concentrated reading, in particular from video display terminals also distinctly reduces the blink frequency and thus the risk for drying an existing tear film out before it is refreshed by a blink.
With the above in mind it is no surprise, that concentrated work at computer screens associated with air condition and low humidity is often associated with a dry eye condition termed as ´office eye´). This affects also younger age groups who are increasingly occupied by concentrated viewing of video-screens of any kind.
A DEFICIENCY IN TEAR FILM FORMATION CAN OCCUR DUE TO EYE LID and BLINKING DYSFUNCTION (LBD) - EVEN WHEN THE TEARS ARE SUFFICIENT
Important for clear vision is not only that we have quantitatively enough tears with qualitatively correct composition. This is not even good enough for an intact ocular surface and for a clear cornea.
During the eye BLINK the upper lid moves over the cornea and conjunctiva. In the down-phase the ´old´tear film is compressed and in the up-phase a new thin pre-ocular tear film is spread over the bulbar surface. This schematic drawing greatly exaggerates the thickness of the tear film in order to make it visible at this enlargement. The tear film thickness is presently found to be typically under the height of one conjunctival epithelial cell.
The formation of the thin pre-ocular Tear FILM is produced by the blink movement of the eye lids, when the upper eye lid spreads out a new tear FILM while it moves back up after a typically short eye closure.
The relatively fragile film must be frequently renewed because it is unstable. It is renewed typically every ten seconds by a new eye blink.
A deficiency in Tear Film Formation even from sufficient tears, can therefore occur when the eyelid function is altered in any way.
This constitutes a deficiency that members of the Ocular Surface Center Berlin have termed as Eye "LID and BLINKING DYSFUNCTION", abbreviated as LBD.
The terminology is inline with other types of tear deficiency, such as Meibomian Gland Dysfunction (MGD) and Lacrimal Gland Dysfunction (LGD).
During the Eye BLINK mainly the upper lid moves vertically over the cornea and conjunctiva. During the down-phase the ´old´tear film is compressed towards the lower eyelid. During the up-phase a ´new´ fresh thin pre-ocular tear film is spread over the bulbar surface.
Dysfunction of the eye lids can also be quantitative and qualitative – similar to the glandular secretion
The Intact Function of the Eye Lids for BLINKING is necessary to transform a sufficient volume and quality of secretion by the Ocular Surface Glands into a Tear FILM. This is required for permanent moisture for maintenance of the integrity of the ocular surface tissue and certainly also necessary for refraction of light in order to provide perfect vision.
A QUANTITATIVE deficiency occurs when the eye lids and blink movement are morphologically intact and produce a sufficient tear film but the frequency of blinking is too low.
Too low means, that the blink interval is longer than the stability of the produced tear film- this is basically described by the concept of the ocular protection index.
The tear film is considered as normal when it is stable for at least 10 seconds. In order to get on with a such a borderline normal tear film the blinking must occur at least every 10 seconds, or 6 times or more per minute.
In line with this, the normal blink frequency is typically given as 5 to 10 times a minute.
The nervous system regulates not only the frequency of the Eye BLINK but also its ´fullness´, which refers to a full closure of the eyelids before they open again, so that the complete pre-ocular tear film can be renewed. So, in a way, the Tear Film is slave to the rhythm of the blink ... as long as the eyelids are principally intact.
In concentrated visual tasks the blink frequency can become so low that it can lead to a Dry Eye condition
In concentrated visual tasks however, particularly in video display terminal work of any kind, including all the laptops, tablet computers and smartphones that we nowadays have everywhere, the blink frequency becomes typically low and easily falls under the duration of tear film stability.
This explains why a dry eye condition, termed "office eye" can easily occur in this condition. Further influence factors on the frequency and effectiveness of blinking can be neurological problems of lid muscle innervation and coordination.
Eye Lid Deformations can impair an efficient eye blink
A QUALITATIVE deficiency occurs when the eye lids and blink movement are morphologically NOT intact. This may typically arise during the normal aging process but can also occur due to trauma, neoplasm, inherited or other diseases.
Morphological lid alterations can occur as part of the normal aging process by a laxity of the eye lids due to decreased elasticity of connective tissue. This leads to Ectropion where parts of mainly the lower lid are no longer fully in touch with the globe. The lower eye lids can thus no longer stabilize the pre-ocular tear film that normally rests on the ´Line of Marx´ of the posterior lid border (for details please see there).
A somewhat ´reverse´ lid condition, Entropion, can also occur due to the aging process. In contrast to ectropion, in entropion the eye lid rolls inward. In addition to dripping of the tears, that can no longer be held at the ocular surface, over the outer lid border, termed epiphora, in entropion the eye lashes typically wipe and scratch on the ocular surface which can distinctly alter the normal structure and cause severe irritation and downstream inflammation (for details please see the section on ´Hierarchy of Pathogenetic Factors´).
CONSEQUENCES of BASIC CAUSATIVE FACTORS are PRIMARY PATHOLOGY of the Tear FILM and Ocular SURFACE
The main PRIMARY Pathologies in Dry Eye Disease are Tear Film Deficiency and Ocular Surface Tissue Damage.
When a dysfunction of gland SECRETION of at least one component - mucins, water or lipids - of the tear film occurs, this leads to Pathology of the Tear Film - termed TEAR FILM DEFICIENCY. This is a PRIMARY Pathology of Dry Eye Disease.
When Tear Film Deficiency exists, this gives rise to sequences of various SECONDARY Pathogenetic Factors such as
Instability of the tear film with
early Break-Up of the tear film and the
formation of Dry Spots at the Ocular Surface.
etc. please see the diagram to the right
SeCondary PathogenETic Factors in Tear Deficiency lead to mechanical friction and hyper-osmolarity of tears.
Tear Film Deficiency typically leads to Damage of the Ocular Surface. This occurs via Sequences of Secondary Pathogenetic Factors in the tear film dynamics that eventually lead to chronic mechanical irritation and hyper-osmolarity.
The secondary alterations of the tear film lead to two main pathogenetic factors:
CHRONIC MECHANICAL IRRITATION
by increased Mechanical Friction due to wetting deficiency with ´dry spots´
HYPER-OSMOLARITY
spots of increased osmolarity
by increased evaporation of the aqueous phase due to a disturbance of the normal tear film structure
Downstream EFFECTS of the main Secondary Pathogenic Factors (Mechanical Friction and Hyper-Osmolarity) are:
both of them lead to cell activation
with up-regulation of inflammatory mediators and
potential onset of inflammatory cascades.
Chronic negative influences decrease the cell viability and eventually lead to cell wounding and destruction.
TISSUE DAMAGE AND TEAR FILM DEFICIENCY ARE BOTH INTIMATELY INTERRELATED AND INTERDEPENDENT
Tear Film and and Ocular Surface Damage are closely interrelated and interdependent - in the normal physiology as well as in pathology. An intact tear film can only bind bind to an intact epithelial surface and the mucosal surface only remains intact when it is permanently kept moist by the tear fluid. In the "typical" Dry Eye Disease that the clinician sees in everyday practice Tear Film Deficiency is typically first and induces Surface Damage - whereas a primary Surface Damage is relatively rare although it may occur in certain conditions.
Thus, a typical downstream effect of Tear Film DEFICIENCY is the onset of Ocular SURFACE DAMAGE of the tissue. This shows how closely the tear film and the ocular surface are interacting and interrelated
In fact the tear film and the ocular surface tissue are interdependent because the moisture of the tears - that can only exist as a tear film in the exposed palpebral fissure - is the pre-requisite for the integrity of the moist mucosal tissue.
And, in return, only an intact mucosal epithelial surface can bind a pre-ocular tear film, which is the pre-requisite for visual acuity ... as explained in the Section for ´Ocular Surface´(for details please see there)
Surface Damage can occur prior to Tear Film Deficiency - but this is rare in typical Dry Eye Disease
A primary Ocular Surface Damage can occur in certain pathologies such as in Vitamin A deficiency. Sin such cases, which are however not what we consider as a "typical" Dry Eye Disease, the Tear Film Deficiency occurs later and secondary to the Surface Damamage.
Squamous Metaplasia is based on a changed epithelial differentiation into a different type of epithelium, with large flat cells and a loss of mucin-secretory goblet cell.
This leads to a mucin deficiency with decreased binding of the tear film to the tissue surface and can thus induces a Dry Eye Disease when it affects larger areas of the conjunctival surface in the palpebral fissure.
In "typical" Dry Eye Disease ... Tear Film Deficiency is first ... and Surface damage occurs downstream and later.
The "typical" Dry Eye Disease is defined by what the doctors see in their daily practice. Most studies on Dry Eye are performed in the reasonably well developed countries, where the individuals have a chance to see a doctor - and reverse.
In countries where a Vitamin A deficiency occurs due to insufficient diet - which tragically still affects many regions of our planet - this is not the case. Vitamin A deficiency inhibits the maturation of the ocular surface epithelium. This results in squamous metaplasia with goblet cell loss and mucin deficiency.
Such patients with dietary Vitamin A deficiency also suffer from Dry Eye Disease, but in these individuals, squamous metaplasia with a primary mucin deficiency constitutes a PRIMARY SURFACE DAMAGE - which is the most frequent underlying cause for Dry Eye Disease here. Tear FILM Deficiency come later in this case.
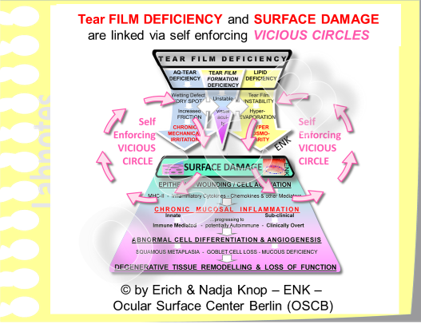
Tissue damage and Tear Film Deficiency are both Primary Pathologies ... and are LINKED via Vicious Circles
Vitamin A deficiency is one example that a primary Surface Damage is possible, other tropic problems e.g. due to pathology of the nervous system would induce similar effects. Such primary Surface Damage will than lead to secondary Tear Film Deficiency. But this is, altogether not the "typical" case in the more developed countries.
Since Surface Damage and Tear Film Deficiency are so closely interrelated, it appears justified and makes most sense from a more general patho-physiological perspective on Dry Eye Disease, when both intimately related pathologies of the Tear Film and Tissue are both designated as "Primary Pathology".
Chronic Inflammatory Pathways are a central component of OCULAR SURFACE DAMAGE
Chronic Inflammatory Pathways are a central component of the disease process of Dry Eye during Ocular Surface Tissue Damage. This is induced by the initial epithelial alterations due to tear film deficiency and may proceed into an immune-mediated mucosal inflammation, if it is not interrupted by therapeutic intervention, to a Degenerative Tissue Remodelling with Loss Of Function.
The initial Surface Tissue Damage that occurs in Dry Eye Disease by wounding and activation of the surface epithelium is the onset of a potential chronic inflammatory process - if this is not timely diagnosed and approached by suitable therapy.
Inflammation is initiated as a very basic protective and repair mechanism that applies tissue degrading enzymes and activates different tissue cells and the vascular endothelium to recruit further cells for help.
Thereby the inflammation tends to proceeds and become more severe,
from a clinical not visible SUB-Clinical Inflammation
into a CLINICAL Inflammation with the cardinal signs of inflammation such as redness, swelling and pain.
KEY events in CHRONIc MUCOSAL Inflammation
Some KEY EVENTS in chronic Ocular Surface Damage of Dry Eye Disease transform the primary protective Repair Mechanism of Sub-Clinical Inflammation into a clinically overt Destructive Chronic Mucosal Immune-Mediated Inflammation
During the chronic inflammatory activity due to the chronic presence of pathogenic stimulation in Dry Eye Disease with presence of tissue wounding and cell activation respective inflammatory mediators accumulate in the tissue with downstream negative effects:
the mucosal immune system can become deregulated and the process transforms into an immune mediated inflammation.
the natural physiological mucosal immune tolerance can be lost and thus
non-pathogenic and environmental antigens but also own tissue antigens can be presented to the resident cells of physiological protective Eye-Associated Lymphoid Tissue (EALT)
with the risk of auto-immune disease.
During the ongoing chronic rounds of inflammation the tissue repair attempts become frustrane and end up in a Degenerative Tissue Remodeling with formation of new blood and lymph vessels with degradation of the collagen matrix and reparative scarring.
Altogether this may eventually end up with a partial or complete Loss of Function of the ocular surface tissue.
VICIOUS CIRCLES typically occur in Dry Eye Disease and give rise to a self-enforcement and worsening of the disease process
Vicious circles are pathogenetic effects, i.e. negative effects promoting the pathology, that act BACK onto themselves and therefore reinforce the disease process.
Often this occurs via the action of interposed further pathogenetic factors and is therefore not always immediately evident at first glance. Vicious circles are not necessarily dependent on inflammation even though an inflammatory process typically gives rise to vicious circles.
As an example, Tear Film Deficiency and Surface Tissue Damage are linked via a Vicious Circle that does not necessarily depend on inflammation. In this pathological reinforcement loop Tear Film Deficiency causes Surface Damage and a damaged Surface is causing more Tear Film Deficiency which will then make the Surface Damage more severe ... and in return.
Such a vicious circle typically goes on and on with progressive worsening of disease until it is eventually recognized and interrupted by a suitable intervention that depends on the nature of the involved factors.
In the Vicious Circle that connects Tear Film Deficiency and Tissue Damage an INTERRUPTION is often possible e.g. simply though the application of suitable tear supplementation in order to decrease friction and normalize a hyper-osmolarity if this exists.
A tear supplementation is however only "suitable" and thus effective when it is patho-physiologically adequate - this means, when it indeed contains the factors that are actually missing.
In the most frequent case of a primary lipid deficiency the tear supplementation should contain lipids and specifically of that type, or, if it exists, another substance with the same action, that is needed to reform a superficial lipid film for retardation of the aqueous hyper-evaporation.