Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT]
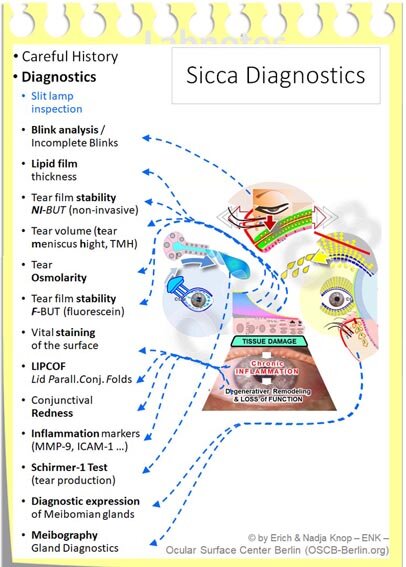
DIAGNOSIS of Dry Eye Disease
This page will deal with:
… A number of examinations and tests for the dry eye that test various functions of the surface of the eye, the tears and the moistening tear film that are used to see whether and to what extent this are intact or disturbed.
=> here is information exclusively about Normal Values of some frequently used clinical test for Dry Eyes
Overview according to FUNCTION of the test
Why is the order of the tests important?
Eyelid tests
In addition to the production of tear fluid, it is extremely important that the tears are spread out into a tear film. This is done by the eyelids and they have several other functions.
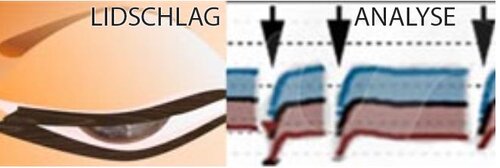
Only a sufficiently frequent and complete eyelid blink is able to produce a stable, even and thin tear film. Any disturbance of the normal eyelid blink can impair the formation of a normal tear film and can thus contribute to Dry Eye Disease.
The eyeblink is certainly influenced by the shape and position of the eyelids but also by neural regulation of the lid muscles.
The shape and position of the eyelids is assessed in the clinical examination - this is done before functional tests
The blinking frequency shows whether the blinking is frequent enough
Completeness of the blink refers to whether the eye is sufficiently closed and thus the entire tear film is renewed
Gland tests
The glands of the ocular surface produce the different components of the tear fluid. The lacrimal gland makes the aqueous tears and the meibomian glands produce oil so that the water does not evaporate too quickly. Meibomian gland dysfunction is currently understood as the most common cause of dry eye.
Lacrimal gland: the SCHIRMER test checks the production volume of the lacrimal gland.
Meibomian glands :
diagnostic expression checks whether they are blocked or open and can give normal oil onto the eyelid margin
the lipid film layer thickness shows the amount of oil on the tear film
Meibography shows potential changes in the glandular structure by meibomian gland dysfunction (MDD) in the living
Tear film tests
These tests check various properties of the tear film that has to keep the surface of the eye moist - always and everywhere. The tear film is the decisive factor that keeps the eye healthy and ensures good visual acuity.
Lipid layer thickness: the thickness of the oil layer on the tear film is important to assess the evaporation of the aqueous tears and the function of the meibomian glands
Tear film stability: is one of the most important parameters for the risk of dry eye. It can be determined by measuring the Tearfilm Break Up Time (BUT)
Tear film osmolarity: with evaporation of the aqueous tears increases their concentration of salts and proteins/ osmolarity which can lead to hyperosmolarity and can damages cells.
Tissue tests / inflammation
Tissue tests check the intactness or damage to the tissue on the surface of the eye. In the case of chronic harmful stimuli, such as in dry eye, the tissue is typically measurably changed. This can provide information about the severity of the disease. Chronic inflammation often develops, causing further damage.
Vital staining is caused by small cell damage (superficial punctate keratitis) on the surface of the cornea and conjunctiva. This occurs for example due to increased friction during dryness and increased osmolarity
LIPCOF ( LIdmargin-Parallel COnjunctival Folds) are based on a loosening of the conjunctiva, which is then raised in wrinkles over the lid margin by mechanical forces. The loosening typically results from chronic inflammation or is at least made worse by it.
Inflammation mediators are typically produced in response to inflammatory stimuli and in dry eye disease and occur in tears and tissues. An important factor is the tissue-resolving enzyme MMP9 (MatrixMetallo Proteinase 9).
Sequence of tests
During the exam, it is important to perform the various tests in an order in which one test does not interfere with the results of subsequent exams.
Tests that consist of pure observations should therefore be carried out first. Meanwhile an increased number of N Non- I nasive ( NI ) tests is available for questions, that could previously only be addressed by invasive tests.
The stability of the tear film, for example
can be done today as an NI-BUT by observing reflections on the surface of the tear film.
the conventional ( F-BUT ) test makes the break-up of the tear film visible by addition of the dye fluorescein. Since this changes the composition of the tear film it may influence the results of later tests. F-BUT is not necessarily less accurate and the previous normal BUT values refer to this test. If the F-BUT test is always carried out in a standardized manner and with little fluorescein, it produces very reliable results and is usually sufficient in clinics.
Below are some important clinical tests arranged in the typical order. By ' clicking ' an image further explanations are available.
The results of the diagnostic tests show which functions are disrupted to what extent and therefore provide information on the degree of severity and which therapy is promising in order to improve the symptoms.
Information about diagnostic tests
Eye LID and BLINKING DYSFUNKTION (LBD) - irregularity of the blinking of the eye
Normal value: ca. 20% of blinks are incomplete (References in Literature differ somewhat)
Pathologic: > 50% incomplete eyelid blinks
The eyelids distribute the tears to the even tear film on the surface of the eyes in the opened eyelid cleft due to the normal complete blinking. The tear film keeps the surface of the eyes moist and is therefore the basis for their health.
Disorders of normal eyelid blinking usually occur:
if the eyelid is changed in shape and position. This occurs especially in old age through sagging of the tissue or with pitted distortions.
if the process of blinking is disturbed - often in the form of an incomplete blink - this is influenced by the neural control of the nervous system
if the frequency is disturbed and blinking typically occurs too rarely (usually with concentrated visual work) - too frequent blinking is less widespread and may be associated with incomplete blinking.
Since the tear film remains stable for only about 10-20 seconds and then breaks-up, it has to be replaced regularly by wiping of the upper eyelid during a blink.
The analysis of an eye blink is not easy clinically ... and is not determined by conventional devices. In addition, the patient should not notice this test because neural influences can then change the blinking behaviour of the eye.
Because incomplete blinking of the eye is inconspicuous, it is typically only detected when is is specifically examined at the slit lamp or, better, by a video recording.
However, this is difficult because the blinking occurs very quickly - moreover, the examination of the blinking is prone to failure and time-consuming. Usual medical devices do not allow automatic examination of the blink pattern and incomplete blinking.
An exception is the LipiVIEW interferometer (from TearScience Inc.), which automatically records the blinking in terms of frequency and completeness when analyzing the tear film lipid layer and the non-invasive tear film stability .
Tear film Lipid Layer (TFLL) Thickness
Normal value: ≥ 65 ICU units (roughly equivalent to 65nm) normal up to about 100 ICU or more - please see image
The oil layer on the outside of the tear film has the function of slowing down the evaporation of the´ tear water´, and thereby keeping the tear film stable over a longer period.
The thickness of the oil layer on the tear film is therefore important for keeping the surface of the eye moist for avoiding a dry eye... and thus ultimately for maintaining ocular health. In addition, as the first light-refractive layer, it is important for perfect visual acuity
Oil deficiency on the tear film, mostly due to obstruction of the meibomian glands in the eyelids, is the presently thought to be the most common cause of dry eye disease.
It is therefore important to determine the thickness of the lipid layer in order to check whether there is a defect that could be responsible for the development of a dry eye.
The thickness of the oil layer can be determined by measuring the interference colors. These are similar to the dazzling colors of an oil stain on a pool of water or to the colors on the surface of a soap bubble. The interference colors are directly related to the thickness of the oil layer, which is in a range of around 100 nanometers, i.e. ten thousandths of a millimeter - that's just as much as the wall thickness of a soap bubble.
With suitable lighting, various diagnostic devices offer the possibility in clinical practice to see the interference colors of the tear film lipid layer.
Detection of the interference colors, that indicate the thickness of the oil layer, is already possible with simple devices that can be connected to an existing slit lamp with little effort.
The exact measurement of the thickness of the lipid layer is possible with the LipiVIEW interferometer. This device determines the thickness very precisely in the range of one nanometer. At the same time, it determines the frequency, pattern and completeness of blinking.
Tear film stability - Non-invasive BUT (NIBUT)
Normal value: ≥ 10 Sekunden
(in NI-BUT the normal values are typically higher, i.e. longer stability, because the tear film is not influenced by addition of a stain. Ni-BUT is simpler to measure, more comfortable and reveals numerical values … it is theoretically more exact)
The tear film break-up time (BUT ) is one of the most important functional values, since an intact tear film is the basis for the moistening and thus for the health of the eye surface.
The BUT describes the time in seconds that the tear film after a complete eyelid blink remains intact, until the first break-up anywhere. When the surface of the eye is intact, the break-up of the tear film is typically the stimulus that triggers a new blink to renew the tear film.
In clinics, the invisible tear film is mainly stained by the vital dye fluorescein (F-BUT) in order to be able to see a break-up. Alternatively there is a non-invasive test to determine the break-up time (NI-BUT) by pure observation without changing the tears film by adding a substance like fluorescein.
The NI-BUT test works by projecting a pattern onto the surface of the tear film and evaluates a certain degree of distortion of the reflected pattern as a breakup.
However, special equipment is required which makes it possible to project onto the surface of the tear film and to monitor the reflection. So-called topographers are often used, who can measure several parameters on the surface of the eye.
Overall, this method promises greater objectivity it
just watch the tear film and
don't change it, moreover it is
in principle faster and
works automatically, providing numerical values
but
it requires a new purchase, unless a topographer or similar already exists
the normal values for the NI-BUT are typically higher (ie longer stability) than for the known F-BUT
it has to be measured several times and then averaged
the accuracy depends on the size of the observation area of the device (whether the entire corneal surface or only the central part is recorded)
Tear Volume / Tear Meniscus Height (TMH)
Normal value: ≥ 0,2 mm
(Height of the tear volume on the ocular surface)
The tear meniscus is the tear lake that forms on the lower and upper ´end´ of the tear film at the contact of the posterior eyelid border with the eyeball (please see image).
Its height is directly related to the actual volume of tear fluid that is present on the eye. TMH thus provides information about the current moistening of the eye.
TMH is not to be confused with Schirmer´s test that instead measures the production of tears by the lacrimal gland !
The amount of tears can in principle not only be determined by the height but also by the curvature / radius of the tear meniscus.
Measuring the height is easier, which is why this is currently the standard method. The normal value for the meniscus height is at least 0.2 mm.
However, the amount of tears does not provide any information about their composition, i.e. the quality.
It is also not clear from the tear meniscus whether the amount of tears currently on the eye is
due to the volume of tear production by the gland or
due to a reduced drainage through the draining tear system into the nose or
caused by the influence of evaporation, eg due to lack of oil.
But ... after all ... one typically assumes that with a normal tear meniscus there are probably no gross disturbances of the moistening on the surface of the eye.
Tears osmolarity - Hyperosmolarity
Normal values: ca. 280 - 306 Osmolarity (mOsms/L), Cut-off: 306 mOsms/L
With increasing numerical value also the tear osmolarity increases (concentration of the salts and proteins).
With increased evaporation (blue arrows) of the tear water, the dissolved substances (salts and proteins - in the figure as white balls) are more concentrated. This leads to locally thin with increased salt concentration (hyperosmolarity), and thus to burning eyes and cell damage .
If there is a lack of tear film lipids (usually when the Meibom oil glands in the eyelids are blocked), an oil layer of reduced thickness lies on the tear film. The tear water then evaporates faster.
As consequences:
the amount of tears on the eye is reduced, which typically leads to reduced ´lubrication´ between the eyelid and eyeball in all eye movements and thus increased mechanical friction occurs - additionally
the concentration of dissolved substances in the tears leads to increased osmolarity / hyperosmolarity. This has a harmful water-extracting osmotic effect on the sensitive cells of the ocular surface
Both increased friction and increased osmolarity are inflammatory and can contribute to the progression of the dry eye to a chronic inflammatory disease.
The tear film osmolarity can now be easily measured with a handheld device (TearLab) and sterile disposable measuring heads. The usefulness of this method is assessed differently and the presence of an inflammatory reaction in the dry eye can often be estimated for the experienced clinician by the overall condition of the surface of the eye. In cases of doubt, for example if a moderate clinical finding clearly differs from a patient's strong symptoms, the determination of the osmolarity can be useful.
The interpretation of tear film osmolarity requires a certain background knowledge because not only the absolute value but also differences between both eyes are relevant
Tear film stability - F-BUT (Fluorescein Break-Up Time)
Normal value: ≥ 10 seconds
(F-BUT with fluorescein is the international standard on which the present research is based and can be measured without special equipment)
The break-up of the thin tear film becomes visible when the tears are stained with the fluorescein dye that is observed in blue light. A break-up occurs as a dark area (seen here in the middle of the faint “C” of the OSCB overlay). The break-up of the tear film is the stimulus that triggers an eyelid blink in order to distribute a new tear film.
The tear film break-up time (BUT ) is one of the most important functional values, since an intact tear film is the basis for the moistening and thus for the health of the eye surface. F-BUT
The BUT describes the time in seconds that the tear film after a complete eyelid bink remains intact, until the first break-up anywhere. When the surface of the eye is intact, the break-up of the tear film is typically the stimulus that triggers a new blink to renew the tear film.
The stability of the tear film is usually checked by administering the yellowish-green vital dye fluorescein for the Fluorescein-BUT test (F-BUT). Fluorescein serves to make the surface of the tear film sufficiently visible in order to see a break-up.
The tear film should be stable for at least 10 seconds before it breaks-up. Since the break-up of the tear film, causes drying of the eye surface an appropriate nerve stimulus is sent to the central nervous system. This signal triggers a new blink to the spread of a new tear film.
The stability of 10 seconds means that one has to blink at least 6 times in one minute so that the surface of the eye does not begin to dry anywhere. If the stability is halved to 5 seconds as often seen in dry eye, then one would have to blink twice as often, in this case 12 times a minute in order to keep the surface moist.
Since most patients actually do not manage about 12 blinks per minute, a reduced tear film stability usually leads to partial drying of the eye surface with corresponding complaints of a dry eye.
Vital staining of the surface of the eye makes damage visible
Normal value: “0” - (i.e. a normal ocular surface should have no vital staining micro-defects)
The representation of damage to the eye surface by vital dyes is an essential cornerstone of the diagnosis of the eye surface in general and especially in the dry eye.
Various dyes (mostly fluorescein, more rarely lissamin green are applied directly to the living vital tissue in the clinic on the patient without causing any damage.
The vital dyes only bind to damaged areas, in the case of surface defects, for example due to increased friction in the dry eye. Any tear film disorder can damage the surface of the eye.
The often punctiform coloration in the case of damage corresponds to superficial punctate keratitis. The amount of staining corresponds to the severity of the disorder. The severity can be classified according to the well-known Oxford scheme .
Punctiform staining corresponds in principle to individual damaged cells or groups of cells.
Since vital staining characterizes damage to the ocular surface tissue, it is the ultimate evidence of the severity of dry eye disease. Therefore the grading of vital staining, typically performed along the Oxford Scheme, is most important for evaluation of the disease severity.
Grading of vital staining - the Oxford Scheme
There are various schemes for classifying the color by severity . The ' Oxford scheme ' is currently the most widespread. It evaluates the vital staining in the interpalpebral fissure, namely in 3 areas: on the cornea and on the temporal and nasal conjunctiva (Figure).
There is usually no vital staining on the healthy surface of the eye. The more cells are damaged, the stronger the staining and, accordingly, the degree of a dry eye. According to the so-called ´Oxford scheme´, the examiner divides the severity into 5 groups semiquantitatively on the slit lamp.
These range from ´0´ (normal, no staining) to ´4´ (strong staining over the entire surface). Level 5 is ´more than level 4’. The schematic drawing here (please see image) on the eye corresponds approximately to level 2 (clear staining especially in the lower area, but not over the entire surface).
LId- Parallel COnjunctival Folds ( LIPCOF )
Normal value: “0“ - ( i.e. a normal ocular surface should not have loosened conjunctival tissue that build up folds on the lid margin)
Pathological LIPCOF folds of the conjunctiva are classified by increasing number and size in typically 3 grades (1-3)
Lid Parallel Conjunctival Folds (LIPCOF) are a clinical sign of tissue damage in chronic dry eye disease.
Lid Parallel Conjunctival Folds, abbreviated as LIPCOF, are an important clinical sign of tissue damage in chronic dry eye disease.
LIPCOF folds indicate a loosening of the conjunctival tissue (please see image), termed ´Conjunctivochalasis´ (from the Greek word χάλασις ("chalasis") for loosening).
The conjunctival loosening is caused by the inflammation in chronic dry eye disease. Large quantities of protein-dissolving enzymes are released continuously. These are matrix metalloproteinases (MMP), especially of the type MMP9.
Conjunctival folds are then generated with all movements of the eyeball in relation to the eyelids. Particularly due to the frequent movement of the eyelids over the eyeball during eyelid blinks. The formation of folds is promoted by the increased friction in dry eyes due to the deficient tear film with reduced ´lubrication effect´.
LIPCOF folds appear parallel to the eyelid margin and can be best observed in the temporal position of the lower eyelids. With increasing tissue loosening, the number of overlapping folds and their height increase (see schematic illustration). The degree of LIPCOF can be graded as a clinical sign for the severity of dry eye disease.
Conjunctival redness index
Normal value: ≤ 1 (depends on the actual grading scale of the equipment)
(Increeasing redness of the ocular surface is typically graded by increasing values from 0 to 3. A certain redness is normal since the ocular surface needs a certain normal blood flow)
The conjunctival redness index is a numerical value for the relative reddening of the conjunctiva in various diseases.
A photo of the surface of the eye is taken with a digital camera and the relative redness compared to a normal pale conjunctiva is then automatically determined with software and output as a numerical value.
Dry eyes typically does not have an intense “red eye”, such as e.g. allergic inflammation. Nevertheless, the reddening of the conjunctiva also increases in a chronic dry eye when the inflammatory activity increases.
Even if intense redness is not typical for a dry eye, the objectification of the relative conjunctival blood filling can be a useful additional parameter for comparing different patients with each other and for monitoring the progress of an individual patient.
MMP-9 enzyme test for the detection of inflammation of the ocular surface
Normal value: “Negative”
A positive test indicates a level of destructive enzyme (MMP9) above a threshold that is considered as normal and is regarded to indicate an inflammatory condition.
Inflammatory reactions are an important part of dry eye disease.
By chronic wounding of the tissue in tear deficiency with increased friction on the ocular surface and increased osmolarity of the tear film are inflammatory mechanisms activated. These lead to more and more destruction and degenerative remodeling of the tissue.
Important factors here are inflammatory cytokines (especially IL1, IL6, TNF-alpha) that attract and activate other inflammatory cells. Upregulated adhesion molecules on the vascular endothelial cells direct the immigration of inflammatory cells from the blood. Tissue-resolving enzymes such as matrix metalloproteinase (MMP), especially MMP-9 destroy the tight tissue fabric to "make room" for an effective cellular inflammatory response.
MMP9 is an essential factor in the inflammatory response of the chronic dry eye. By breaking down the normal tissue structure, MMP-9 leads to degenerative tissue remodeling. Such tissue destruction is responsible, e.g. for the loosening of the conjunctival tissues that leads to the formation of LIPCOF folds.
A detection of MMP-9 enzymes in the tissue and tear film is therefore an important diagnostic factor for the detection of sub-clinical inflammation on the surface of the eye. This can be useful for the indication for the implementation of anti-inflammatory therapy in the dry eye.
Previously such investigations were only possible in a scientific laboratory. It has now become possible to carry out MMP9 enzyme detection directly in the practice on the patient by using an MMP protein detection stick (InflammaDry), that works similar to a pregnancy test. The device tip is brought into intensive contact with the tear film and the conjunctiva in the lower fornix and the result can be read within a few minutes by formation of colored lines.
Schirmer´s test for aqueous tear production
Normal value: ≥ 10 millimeter in 5 minutes
(indicates the amount of new tear production as wetted area of a paper strip)
The bent edge of the test strip is inserted into the lower fornix over the lateral third of the lid margin. Then the eyes are largely closed during the 5 minutes of the test.
The Schirmer´s test measures the amount/ volume of aqueous tear fluid newly produced by the lacrimal gland during a period of 5 minutes. The test is usually carried out as a Schirmer-1 test without a local anesthetic in order to check the maximum production capacity of the lacrimal gland.
Schirmer´s test is therefore not to be confused with the tear meniscus height (TMH), that measures the preexisting volume of the tears on the ocular surface and is influenced by various factors.
Procedure
A standardized filter paper strip is hung over the temporal third of the lower edge of the lid (see image). It is typically recommended to close the eyes to a large extend.
Since the filter paper strip represents a certain intended stimulus, the Schirmer 1 test (without local anesthesia) is testing a stimulated secretion - and not a so-called basal tear secretion. Therefore, this test provides information about the maximum performance of the lacrimal glands and thus about is health.
Notes on performance:
In order to avoid absorption of excess tear fluid, that may be present in the lower fornix, it is important to remove such fluid in order to avoid an erroneously high reading.
It is important to bend the test strip correctly and to insert the bent end deep enough into the lower fornix in order to produce the necessary stimulus for the ´stimulated´ tear production. If despite recognizably sufficient tear volume (TMH) on the eye and with a clinically largely intact surface, a tear secretion of "0" is measured - i.e. a practically dry Schirmer strip - then the Schirmer test may be repeated to ensure a correct measurement.
=> HERE is further information about Schirmer-1 and related Tests for tear secretion
Results
The minimum value for aqueous tear production within 5 minutes is usually 10mm wetting distance. Values below this are considered as a too low tear production.
Interestingly enough, many patients with a “dry eye” actually have episodes of excessively high aqueous tear production. This produces wetting values typically well above approx. 20-25 mm. Sometimes the completely strip is soaked with tears. This can be explained by the fact that the so-called 'dry' eye is actually a chronic irritation of the surface of the eye that can lead to a reflex excessive tear production with a ' wet eye '.
Only the relatively rare disorders of the lacrimal gland itself reveal a very low tear production value close to zero in Schirmer´s test. Such disorders are typically inflammatory, for example in the very rare Sjögren's syndrome or in the autoimmune inflammation of graft-versus-host disease (GvHD) after bone marrow transplantation.
Diagnostic expression of the meibomian glands - lipid delivery
Normal value: Meibomian glands yielding liquid secretion (MGYLS)
typically indicated as: (No of secreting glands) ca. 6-10 / 15 (investigated glands)
The simplest test for the effective functionality, i.e. the ´activity´, of a meibomian glands is the technique of diagnostic gland expression. This is a test for the release of already produced oil from the duct system of the meibomian glands onto the eyelid margin.
Diagnostic expression of oil from the Meibomian glands is practically the 'oily equivalent' of Schirmer´s test for aqueous secretion of the lacrimal gland, because:
it tests the availability/ volume of a secretion product on the surface of the eye - in the case of the meibomian glands by testing the release of the oil on the edge of the eyelid.
it also tests the quality of the secretion, i.e. whether the lipids form a normal clear oil, are cloudy, contain granules or have a toothpaste-like condition.
The diagnostic expression of the meibomian oil is carried out by very mild pressure, for example with the finger on the outside of the eyelid margin (please see image) - such as through muscle contraction during normal blinking.
In order to maintain the very mild pressure (1.25g per mm2) that arises with normal blinking, a standardization was achieved by Donald Korb, Boston. He constructed a small hand-held instrument - the MGE, Meibomian Gland Evaluator (TearScience Inc, JnJ). This is a very useful little instrument for those who are really interested in dry eye disease and Meibomian gland dysfunction (MGD).
The MGE generates exactly the defined pressure onto an area under which about 5 meibomian glands are located. In this way, 5 meibomian glands are tested together in a standardized way in each lower eyelid to get an idea of the condition of the meibomian glands and their oil formation.
In order to standardize diagnostic expression even more, the expression must always be performed in the same 3 locations along the eyelid margin, i.e. in the nasal, medial or temporal part of the lower eyelid margin. This is important as it was observed by Blackie and Korb that the activity of the Meibomian glands have typically different activity in the different locations along the lid margin. Best is of course if all three locations are tested in every patient and the respective results compared.
Investigated glands: 5 glands each in 3 locations (nasal, medial, temporal) along the lid margin makes 15 glands that are evaluated. The evaluation reveals the “Meibomian gland score” that consists of different parameters as shown below:
Meibomian gland score
MGYLS (liquid secretion)
Often performed test: Only the number of meibomian glands yielding liquid secretion (MGYLS) is evaluated among the 15 glands along each eyelid as described above. This refers to glands that reveal any liquid secretion - either clear or cloudy. Toothpaste like secretum is therefore excluded.
Optimal Clear secretion
More focused is the recording of only those glands that yield an optimal clear liquid oil, which excludes already those glands that produce cloudy oil.
Total Meibomian gland score reveals more detailed information
= sum of the factors for all 15 investigated glands along each lid margin (result: 0 to 45)
Secretion Characteristics factor
clear liquid secretion (3)
cloudy liquid secretion (2)
inspissated/toothpaste-like (1)
no secretion (0)
Meibomian gland structure can be depicted in the eyelid by meibography
Normal value: “0“
Display of the Meibomian gland mass in the eyelids: Classification from “0“ Normal (all glands are present) along progressive loss of one thirds on the glands each in the grades 1-3. In grade 3 = loss of 3/3 of glands (i.e. practically no more glands present)
Meibography allows to display the structure of the meibomian glands inside in the patient's eyelid directly in the doctor's practice.
This is a valuable technique
Diagnostics: - to assess the state of the meibomian glands in patients with dry eyes. It is important to find out whether obstruction of the meibomian gland ducts and openings has already caused damage to the gland tissue by the permanently increased pressure. Such morphological investigation may also document potential improvements of gland structure if they occur in the course therapy.
Education: - it is instructive for patient guidance to show directly the realistic image of their meibomian glands. The structure can be related to the symptoms of dry eye disease and make them more understandable. It is also useful to show, how important e.g. a consistent local physical eyelid margin therapy is for the improvement of the disease condition. Or, alternatively, to explain the rationale for a more effective apparative therapy in the eye doctor´s practise with e.g. the Lipiflow automatic physical therapy device.
The glandular tissue is typically visualized by illuminating the glands from the inside of the eyelid. The glands appear bright in the infrared light. However, the representation of the meibomian glands is not easy, since the surface of the eye is a natural "wet area" - a mucous membrane. The moist surface produces many reflections when illuminated.
Disturbing reflections therefore typically occur on most meibography images and it takes a certain degree of experience of the examiner and can be time-consuming to keep the reflections as low as possible. This is a prerequisite for a meaningful image for the clinical documentation.
A photo production with perfect contrast and resolution allows the meibomian glands to be displayed as if they were openly exposed and not covered by the overlying tissue of the lid plate and the conjunctiva. As a result, the structure of the glands is immediately recognizable by the doctor ... and also by the patient.
The perfect and undisturbed display of such difficult objects as the meibomian glands requires sophisticated systems for lighting and for electronic image processing. Both must be combined in order to achieve perfect image quality. There is currently only one device type that meets these requirements and therefore allows meibomian glands to produce images of unprecedented clarity and precision in almost histological resolution - the Lipiview and the Lipiscan (from TearScience Inc.,, nowJnJ).