Dry Eye Concept 6 -
HIERARCHY of Pathogenetic Factors
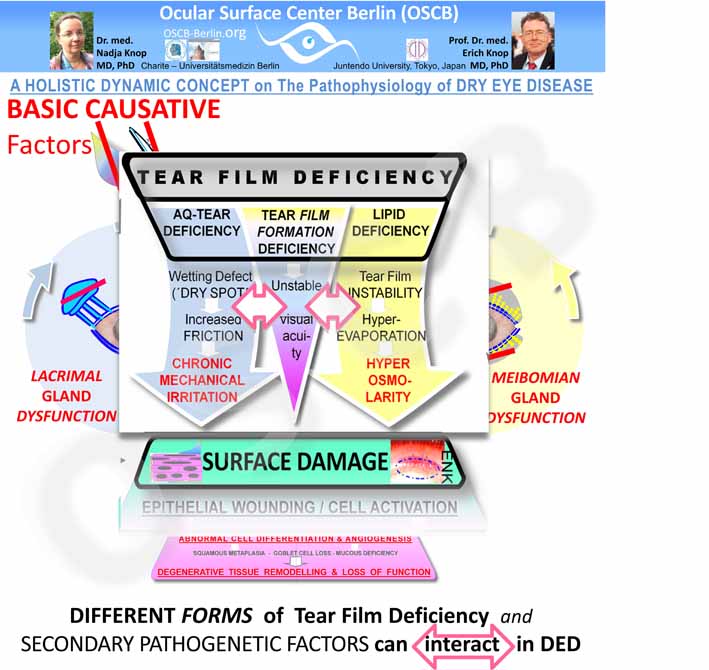
Pathogenetic Hierarchy: CAUSATIVE FACTORS cause PRIMARY PATHOLOGY ... that is governed by Sequences of Secondary Pathology
... ouuups ... that sounds complicated again - don´t worry just follow the tour !
As explained in the previous Section:
- 1. BASIC FUNCTIONAL COMPLEXES are those that are necessary to provide MOISTURE at the Ocular Surface - everywhere & every time ... which is maintained by:
- SECRETION of tear components by the glands.
- Rationale: no liquid - no moisture
- Tear FILM FORMATION
- Rationale: no FILM of tears => no permanent moisture in the palpebral fissure => no health of the tissue
- SECRETION of tear components by the glands.
- 2. CAUSATIVE FACTORS come into existence then the basic functional complexes fail
- Failure/ LACK of basic functions means: onset of pathology !
- 3. PRIMARY PATHOLOGY in Dry Eye is what is known to every clinician:
- Tear FILM DEFICIENCY
- SURFACE DAMAGE
Primary Pathologies are governed by SEQUENCES of SECONDARY PATHOGENIC Factors that drive the Disease process
Sequences of secondary pathogenic factors
that occur downstream to the primary pathology
govern the pathological process
and thus lead to disease progression and worsening of the condition.
Secondary Pathogenetic Factors in Tear Film DeficieNCy
Sequences of Secondary Pathogenetic Factors govern the primary pathology of Tear Film Deficiency - and interact with each other. The secondary pathology terminates in Chronic Mechanical Irritation by Friction and Hyper-Osmolarity as the main factors that induce Damage of the Surface Tissue.
Tear Film Deficiency gives rise a sequence of various Secondary Pathogenetic Factors. Examples are known to most clinicians and encompass factors such as:
- instability of the tear film with early Break-Up
- formation of Dry Spots at the Ocular Surface
- increased friction
- chronic mechanical irritation
- hyper-evaporation
- hyper-osmolarity of the tear film
Allocation of individual secondary pathology to specific types of tear film deficiency is difficult
This very schematical diagram is supposed to indicate that the Different Types of Tear Film Deficiency that determine the Type of Dry Eye Disease tend to mix with increasing severity of disease. This is conceivably due to the impairment of more and more functional complexes with downstream negative effects as the disease process proceeds, destroys for tissues and becomes more severe.
It is difficult to allocate such secondary pathology to specific types of tear film deficiency.
- Lipid deficieny is e.g. typically discussed together with
- tear film instabilty which is then though to be
- linked to hyper-evaporation of the aqueous phase which is reason for
- hyper-osmolarity of the the tear film
- On the other hand, in aqueous deficiency
- wetting defects are often discussed in the context of the
- formation of dry spots as regions where
- increased friction due to
- decreased lubrication occurs which eventually leads to
- chronic mechanical irritation.
In fact, the factors in secondary pathology are interacting - which is indicated in the Dry Eye concept by horizontal white arrows linking the different types of tear film deficiency.
Since secondary pathogenetic factors interact anyway, it is probably not too surprising that it is difficult to clearly allocate them.
There is also some indication, reported by BRON and LEMP, to think that different types of Dry Eye Disease may only be clearly discernable in initial phases of Dry Eye.
Whereas during the progression of Dry Eye Disease of the typically chronic disease process the individual disease types tend to mix progressively as the disease progresses and affects more functional circuits with accumulating and overlapping pathology.
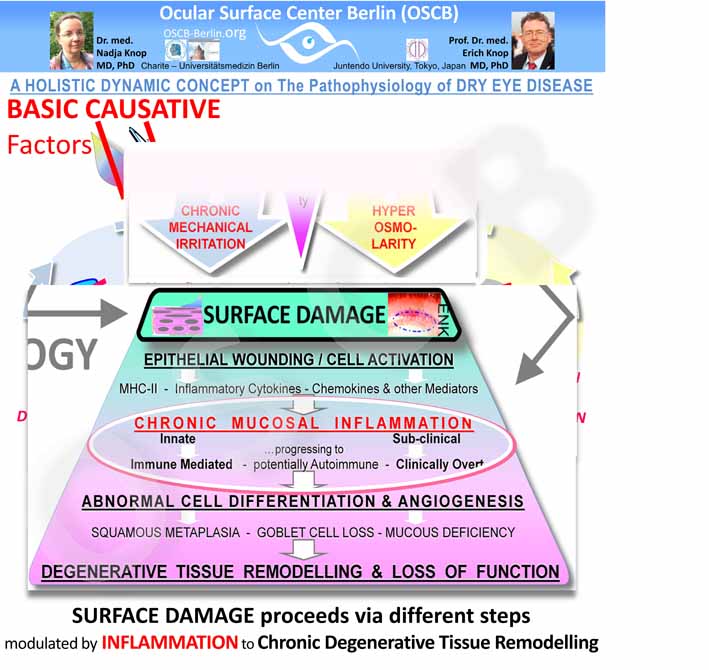
Secondary Pathogenetic Factors in Ocular Surface TISSUE DAMAGE reflect aspects of Inflammatory Cascades
Secondary Pathogenetic Factors in SURFACE Tissue DAMAGE also form Sequences of increasing severity that propagate the disease process. Chronic inflammation is the main amplifier of disease - it gives rise to several Vicious Circles and to a Chronic Tissue Remodeling with Loss of Function.
The secondary pathogenetic events that occur in SURFACE TISSUE DAMAGE reveal characteristics of pathways of chronic mucosal inflammation.
Apparently the primary impact is on the epithelial cells of the cornea and conjunctiva - which is in line with the observation that an insult typically comes from the outside, i.e. the luminal region, i.e. here the tear film - even though pathology can also start in the tissue, as discussed above.
Chronic alteration of epithelial cells at the Ocular Surface induces a Chronic Inflammatory Process
Inflammation as such is no major problem in principle because it is a very basic protective answer of tissues to many noxious stimuli that intends to remove the negative stimulus. Inflammation is a regulated process and thereby limited - it typically ends with a regeneration, repair and healing.
A schematic mechanistic diagram shows some KEY EVENTS in Mucosal Inflammation during Dry Eye Disease
However, a single vicious circle is misleading - it is half true and half wrong ... such ideas usually cause most problems.
Inflammatory processes are typically first innate and subclinical - which means it does not, or very limited, show the typical clinical signs of inflammation such as redness, swelling, heat and pain.
Therefore the impression that such signs are absent in patients does not tell there is no inflammation of any degree.
Chronic sub-Clinical inflammation proceeds to immune-modulated inflammation
Inflammation becomes problematic
- when it becomes chronic - and therefore unlimited - and
- when an innate inflammation involves the specific immune system to turn into an immune-mediated inflammation - which can strongly amplify the inflammatory process and
- when a further transformation of the immune-mediated inflammation into an auto-immune disease may occur
At the ocular Surface in Dry Eye Disease unluckily, but typically, two of these problems exist - chronicity and immune-modulation. Auto-immune disease in Dry Eye is presently only shown in a mouse model by NIEDERKORN and colleagues but may also be possible in the human.
The CHRONIC INFLAMMATION in Dry Eye Disease includes
as described in the diagram to the right - taken from a paper by Members of the Ocular Surface Center Berlin (OSCB) in the journal ´The Ocular Surface´2005:
- the CHRONICITY of the tissue irritation
- when the deficiency of the tear film persists or even becomes worse due to the interdependence of the integrity of tissue and tear film
- the wounding and ACTIVATION of cells with a build-up of an INFLAMMATORY micro-milieu. Downstream events are:
- up-regulation of adhesion molecules on vascular endothelial cells & recruitment of lymphoid cells from the vascular compartment
- up-regulation of antigen-presentation molecules and co-stimulatory molecules
- aberrant antigen-presentation due to the continuous presence of inflammatory danger signals that can deregulate antigen-presentation
- presentation of auto-antigens from own cells to lymphoid cells in the context of inflammatory danger signals that can lead to auto-immunity.
- activation of proteases (Matrix-Metalloproteinases, MMPs) that degrade the connective tissue stroma.
Chronic Inflammation results in downstream secondary pathogenetic factors such as:
- abnormal cell differentiation with squamous metaplasia,
- loss of goblet cells and their mucins
- thus a loss of surface wettability
- leading to increased tear film instability
- neovascularization with formation of new blood and lymph vessels that
- destroy the corneal transparency
- drive the recruitment of more lymphoid cells and other leukocytes
- drives the inflammation
- impairment of normal cell differentiation that contributes e.g. to squamous metaplasia and loss of mucins
- chronic cycles of inflammatory destruction of the connective tissue to provide space of an effective inflammation that run in parallel with frustrane repair mechanism with formation of scar tissue - this leads to Degenerative Tissue Remodeling
Chronic inflammation is an important factor for amplification of the disease process in Dry Eye
In a worst case scenario, such chronic ocular surface inflammation can lead to Degenerative Tissue Remodeling with Loss of Function as shown in the mechanistic diagram.